Pre-existing condition coverage ensures individuals with prior health issues receive necessary medical care without discrimination, while essential health benefits mandate a standardized set of health services covered by insurance plans, promoting comprehensive care for all enrollees. Understanding the distinctions between these coverage types is crucial for selecting the right insurance plan. Explore more to make informed health coverage decisions tailored to your needs.
Why it is important
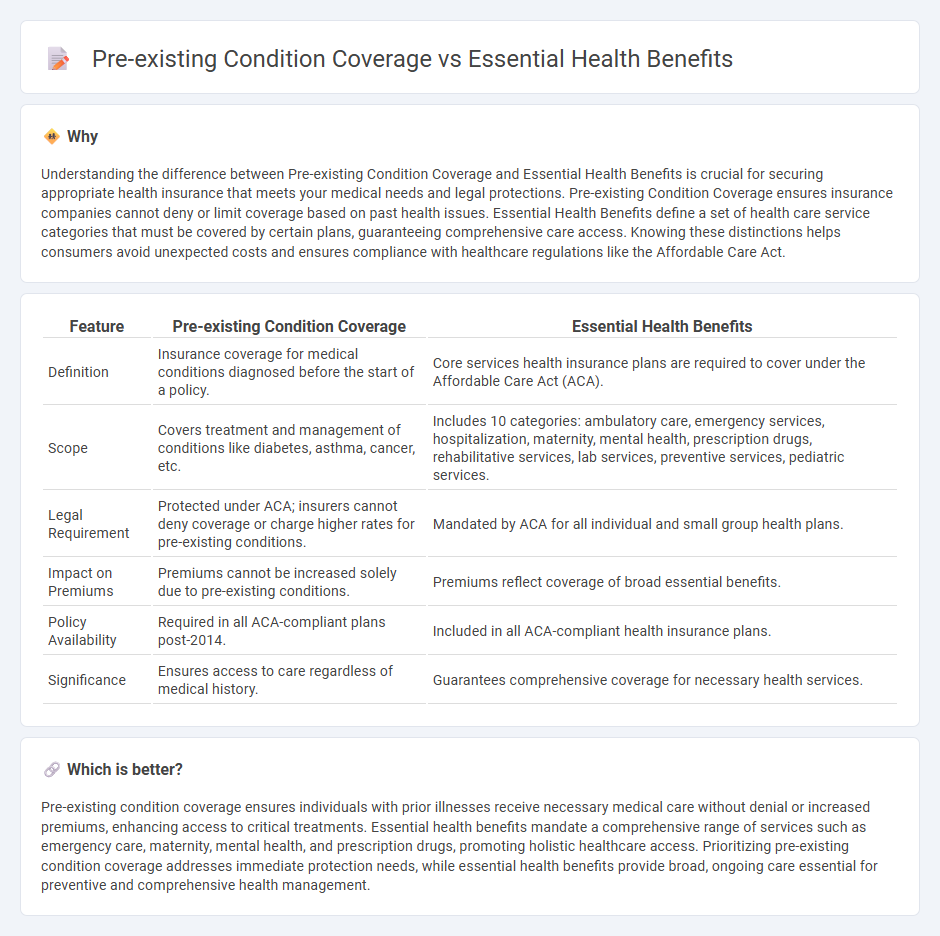
Understanding the difference between Pre-existing Condition Coverage and Essential Health Benefits is crucial for securing appropriate health insurance that meets your medical needs and legal protections. Pre-existing Condition Coverage ensures insurance companies cannot deny or limit coverage based on past health issues. Essential Health Benefits define a set of health care service categories that must be covered by certain plans, guaranteeing comprehensive care access. Knowing these distinctions helps consumers avoid unexpected costs and ensures compliance with healthcare regulations like the Affordable Care Act.
Comparison Table
| Feature | Pre-existing Condition Coverage | Essential Health Benefits |
|---|---|---|
| Definition | Insurance coverage for medical conditions diagnosed before the start of a policy. | Core services health insurance plans are required to cover under the Affordable Care Act (ACA). |
| Scope | Covers treatment and management of conditions like diabetes, asthma, cancer, etc. | Includes 10 categories: ambulatory care, emergency services, hospitalization, maternity, mental health, prescription drugs, rehabilitative services, lab services, preventive services, pediatric services. |
| Legal Requirement | Protected under ACA; insurers cannot deny coverage or charge higher rates for pre-existing conditions. | Mandated by ACA for all individual and small group health plans. |
| Impact on Premiums | Premiums cannot be increased solely due to pre-existing conditions. | Premiums reflect coverage of broad essential benefits. |
| Policy Availability | Required in all ACA-compliant plans post-2014. | Included in all ACA-compliant health insurance plans. |
| Significance | Ensures access to care regardless of medical history. | Guarantees comprehensive coverage for necessary health services. |
Which is better?
Pre-existing condition coverage ensures individuals with prior illnesses receive necessary medical care without denial or increased premiums, enhancing access to critical treatments. Essential health benefits mandate a comprehensive range of services such as emergency care, maternity, mental health, and prescription drugs, promoting holistic healthcare access. Prioritizing pre-existing condition coverage addresses immediate protection needs, while essential health benefits provide broad, ongoing care essential for preventive and comprehensive health management.
Connection
Pre-existing condition coverage prevents insurers from denying or charging higher premiums to individuals with prior health issues, ensuring access to necessary care. Essential Health Benefits (EHBs) guarantee that plans provide comprehensive services like hospitalization and prescription drugs, crucial for managing chronic conditions. Together, they create a safety net that promotes affordability and comprehensive treatment for individuals with pre-existing conditions.
Key Terms
Coverage requirements
Essential health benefits mandate coverage of a core set of services including ambulatory care, emergency services, hospitalization, maternity care, and prescription drugs, ensuring comprehensive access to necessary medical treatments. Coverage for pre-existing conditions prohibits insurers from denying or limiting benefits based on an individual's health history, guaranteeing continuous care regardless of prior health issues. Explore more about how these coverage requirements protect consumer health rights and promote equitable access to healthcare.
Eligibility
Essential health benefits refer to a set of 10 categories of services, such as emergency care and prescription drugs, that health insurance plans must cover under the Affordable Care Act. Pre-existing condition coverage guarantees that individuals with prior illnesses or health issues receive insurance without denial or extra charges, ensuring continuous healthcare access. Explore how eligibility criteria affect these protections to better understand your health plan options.
Benefit limitations
Essential Health Benefits (EHB) define a set of ten categories of services health insurance plans must cover under the Affordable Care Act, including preventive, emergency, maternity, and mental health services, ensuring comprehensive care. Pre-existing condition coverage guarantees that individuals with health conditions diagnosed before their insurance enrollment cannot be denied coverage or charged higher premiums, though some plans might impose benefit limitations like treatment caps or network restrictions. Explore how benefit limitations impact your access to care and costs by reviewing detailed plan comparisons and regulatory updates.
Source and External Links
What are essential health benefits? - Essential health benefits are ten categories of services that all new individual and small-group health insurance plans must cover under the Affordable Care Act, including hospitalization, prescription drugs, ambulatory services, emergency services, maternity care, mental health, lab work, preventive services, pediatric dental and vision care, and rehabilitative services, with no annual or lifetime spending limits by insurers.
Essential health benefits - Defined by the ACA, essential health benefits are ten mandatory insurance coverage categories such as ambulatory care, emergency services, hospitalization, maternity, mental health, prescription drugs, rehabilitation, laboratory services, preventive care, and pediatric services including oral and vision care.
10 Essential Health Benefits Insurance Plans Must Cover ... - ACA mandates that all individual and small group health plans cover ten essential health benefits including outpatient services, emergency care, hospitalization, maternity, mental health, prescription drugs, rehabilitation, lab work, preventive wellness, and pediatric oral and vision care to ensure comprehensive patient coverage.
 dowidth.com
dowidth.com